
Various imaging studies can be used to evaluate patients with suspected renal or urinary tract disease. [1] Renal angiography is the gold standard for direct visualization of the renal vasculature. It is invaluable in the diagnosis and prognosis of renal artery stenosis and renal vein thrombosis. [2] Plain films of the abdomen are now rarely used to evaluate kidney and urinary tract disease. Renal ultrasonography is invaluable as a screening test for urinary tract dilatation (hydronephrosis), a hallmark of urinary tract obstruction. Ultrasonography remains the procedure of choice for evaluation of acquired or hereditary polycystic kidney disease. [3] Color doppler ultrasonography is used to measure flow or velocity of blood in the main renal artery; it is primarily used to detect renal vascular occlusive disease. [4, 5, 6, 7]
Plain abdominal films are indicated for the evaluation of radiopaque kidney stones (calcium-containing stones, struvite, cystine). An advantage of the plain film is that it can be performed in pregnant and pediatric patients, since the amount of radiation exposure is limited.
Intravenous pyelography (IVP) can be used to detect kidney stones and delineate the level of obstruction in patients with urinary tract obstruction.
Computed tomography (CT) is an excellent tool to evaluate masses, traumatic injury to the kidney, stones, and pyelonephritis. CT scanning is superior to ultrasonography in identifying renal cysts, since it is capable of detecting small cysts (2-3 mm in diameter). [5, 6]
Magnetic resonance imaging (MRI) provides a useful alternative to CT scanning in individuals at risk for toxicity from intravenous contrast.
Radionuclide scanning has been successfully used to evaluate renal perfusion in various settings, including renal artery stenosis and thrombosis. Radionuclide cystography is widely used by pediatric nephrologists to detect early vesicoureteral reflux in children. [8]
Retrograde pyelography is an essential tool for localizing the site of urinary tract obstruction. It has been replaced by ultrasonography or CT scanning in most settings but is helpful in patients with a known pelvic malignancy when hydronephrosis is absent because of ureteral encasement. [9]
Diuretic renography is widely used to discriminate functional versus anatomic obstruction after identification of a dilated upper urinary tract (usually with ultrasonography or CT scanning). [10] Two important functional aspects of kidney function can be assessed: (1) clearance of each kidney and (2) the flow of urine through the urinary tract.
Plain films of the abdomen are now rarely used to evaluate kidney and urinary tract disease. Plain abdominal films are indicated for the evaluation of radiopaque kidney stones (calcium-containing stones, struvite, cystine). An advantage of the plain film is that it can be performed in pregnant and pediatric patients, since the amount of radiation exposure is limited. (See the image below.)

--> Plain film of the abdomen revealing a radiopaque staghorn calculus involving the entire pelvicalyceal system of the right kidney (arrows). This stone was composed of magnesium ammonium phosphate (struvite). Surgical excision, antimicrobial treatment, and consumption of 4-5 L/d of water are all required to treat and prevent this type of stone.
The sensitivity and specificity of plain abdominal films in detecting a stone is low in patients with renal colic and no history of kidney stones. [1] However, plain films can be used for follow-up of stone clearance, growth, or recurrence after operative or conservative treatment of stones.
It is difficult to distinguish vascular calcifications from ureteral calcifications with plain radiography. Because of its higher sensitivity, CT imaging has replaced plain films for the diagnosis of urolithiasis and nephrolithiasis. [11]
Plain films are not sensitive enough to exclude tumors of the kidney or urothelial tract. This imaging technique does provide general information regarding kidney size and shape.
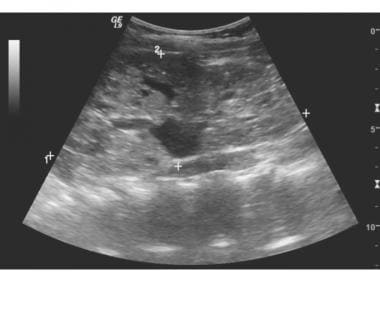
Renal ultrasonography is invaluable as a screening test for urinary tract dilatation (hydronephrosis), a hallmark of urinary tract obstruction. However, dilation of the urinary tract may also be observed in polyuria and normal pregnancy (uterine enlargement causes partial urinary tract obstruction). Urinary tract dilation may persist indefinitely, even after relief of urinary tract obstruction. Parapelvic cysts may also be mistaken for pelvocaliectasis. [2, 4, 12, 7]
Indications for renal ultrasonography include the following [1] :
Evaluation of cystic kidney disease. Diagnosis of hydronephrosis. Measurement of kidney size and echogenicity as part of an evaluation of chronic kidney disease. Detection of renal artery occlusive disease via Doppler images. No exposure to radiation or contrast in pregnancy.(See the image below.)

--> Sonogram revealing a dilated collecting system caused by an enlarged lymph node in a patient with B-cell lymphoma.
Ultrasonography remains the procedure of choice for evaluation of acquired or hereditary polycystic kidney disease. [3] Renal masses are also readily identified with ultrasonography. [13] Advanced kidney disease is usually accompanied by scarring and thinning of the renal cortex with small kidneys (< 9 cm in longitudinal length). These features are easily characterized with renal ultrasonography. [12, 14] (See the image below.)
--> Numerous cystic structures are evident on the renal sonogram.
Although renal ultrasonography was once routinely used to identify kidney stones, noncontrast helical computed tomography has supplanted ultrasonography in the diagnosis of nephrolithiasis.
Color Doppler ultrasonography is used to measure flow or velocity of blood in the main renal artery. It is primarily used to detect renal vascular occlusive disease. [4] Color Doppler flow studies in the renal artery are highly operator-dependent.
Indications for IVP include delineation of the gross anatomy of the renal and urinary tract and evaluation of medullary sponge kidney and papillary necrosis. Avoid IVP in patients with allergy to iodine contrast dye and in patients with impaired renal function (generally a serum creatinine level >2 mg/dL). IVP was the earliest imaging technique to define the anatomy of the renal and urinary tract using iodinated contrast injection, which is excreted by the kidneys into the collecting system.
IVP can be used to detect kidney stones and delineate the level of obstruction in patients with urinary tract obstruction. The acquisition of data is slower than with other forms of imaging (eg, CT scanning). In pregnant patients, IVP with limited contrast can be performed if ultrasonography is unrevealing. IVP is an excellent modality to diagnose medullary sponge kidney and papillary necrosis.

--> Intravenous pyelogram in a patient with medullary sponge kidney. Note the brushlike pattern (arrows) involving the renal papillae. This pattern is consistent with numerous ectatic medullary collecting ducts and is pathognomonic for medullary sponge kidney.
Computed tomography (CT) provides similar information as renal ultrasonography but with additional detail because of high spatial resolution. Indications for CT scanning include nephrolithiasis, kidney masses, traumatic injury to the kidney, staging renal tumors, polycystic kidney disease, and pyelonephritis. [5, 6, 7]
The primary limitation of CT scanning is the risk of radiation and administration of contrast. Contrast should be avoided if the patient is allergic, has renal failure, or is pregnant. In the precontrast phase, a scan is obtained for baseline calcifications, stones, and space-occupying lesions in the kidney and urinary tract. Within 70 seconds after injection of contrast, the renal vasculature is identified and renal cell carcinoma can be accurately staged. In the nephrographic phase (ie, up to 180 seconds after contrast injection), renal masses can be differentiated from simple cysts, as malignant masses will enhance with contrast. In the excretory phase (5 minutes after contrast injection), the ureter, bladder, and pelvicaliceal system is imaged. Limited CT urography (with an excretory phase only) can be performed to minimize radiation exposure.
No preparation is required, but prehydration is typically performed, and the bladder should be empty before the procedure is begun. Intravenous saline administration or administration of 10 mg of intravenous furosemide is often used to increase opacification and distention of the collecting system.
The supine position seems to be satisfactory in most patients, but the prone position improves opacification of the distal urinary tract in some patients. Turning the patient several times before the excretory phase is necessary to prevent layering of contrast.
(See the image below.)
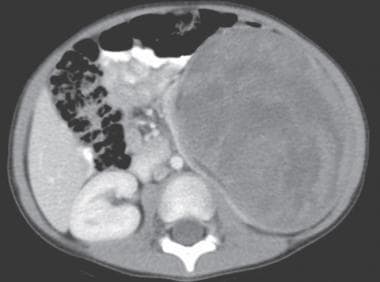
--> CT scan reveals an enormous, contrast-enhanced mass in the right kidney of a patient with Wilms tumor. The mass consists of several hypodense areas most likely reflecting necrosis or hemorrhage.
Noncontrast helical CT scanning is the procedure of choice to evaluate kidney stones. [15] CT scanning is also used to differentiate malignant from nonmalignant renal masses. [13] Moreover, CT scanning is essential to evaluate the local spread of a renal malignancy. High-resolution CT angiography is excellent in defining the anatomy of the renal arteries and veins (eg, renal vein thrombosis).
(See the image below.)
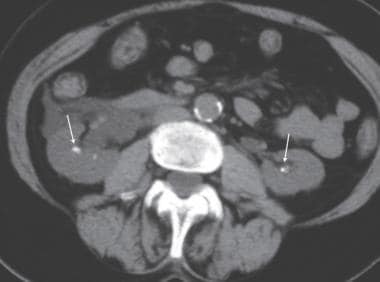
--> Helical CT scanning in a patient with hematuria. Nonenhanced CT image shows bilateral renal calculi (arrows). This imaging technique is considered the reference standard for stone evaluation.
CT scanning is superior to ultrasonography in identifying renal cysts, since it is capable of detecting small cysts (2-3 mm in diameter).
CT of the abdomen and pelvis is usually appropriate for imaging acute pyelonephritis in patients with diabetes, patients who are immunocompromised, and patients with a history of stones or renal surgery. [16]
Because of safety and cost, renal ultrasonography is still used to screen for polycystic kidney disease.
(See the image below.)

--> Computed tomography scan of autosomal-recessive polycystic kidney disease revealing many small cysts. Note the small cyst in the head of the pancreas (arrow). RK = right kidney.
With the advent of multidetector CT scanning, CT urography is a feasible option to replace intravenous urography.
Multiphase CT urography [17] has a higher diagnostic yield in evaluating the etiology of hematuria and identifying urothelial tumors than intravenous urography. Some investigators believe it is comparable to cystoscopy and provides complementary data by simultaneously delineating extraurinary disease.
Magnetic resonance imaging (MRI) provides a useful alternative to CT scanning in individuals at risk for toxicity from intravenous contrast. It may also offer an advantage in the evaluation of small renal masses. Magnetic resonance angiography has proven to be useful in the evaluation of stenosis in the mid and proximal renal arteries.
T2-weighted magnetic resonance techniques rely on high signal intensity of urine for image contrast. Images can be obtained quickly and in any image plane. The images are appealing when compared to intravenous urography. The signal-to-noise ratio (SNR) is increased with phased-array surface coils to achieve maximal interpretable resolution. A further increase in SNR is achieved by imaging with higher field strength; however, this also increases susceptibility artifacts from gas-filled bowel, and this technique therefore needs further investigation.
Indications for MRI include the following:
Detailed assessment of the kidney anatomy Noninvasive assessment of kidney function Estimation of GFR [18] Magnetic resonance renography [19] Assessment of congenital anomalies of the kidney, bladder, and urinary tractProgressive systemic fibrosis (nephrogenic systemic fibrosis [NSF]) in patients with kidney failure has been recognized. This disorder has been reported only in patients receiving gadolinium, a contrast agent used to enhance the standard MRI. Therefore, MRI with gadolinium contrast is typically avoided in patients with a serum creatinine level exceeding 2 mg/dL (estimated glomerular filtration rate [eGFR] < 30 mL/min), unless deemed urgent, and postexamination dialysis may be indicated in selected cases.
Magnetic resonance renography (MRA) has shown promising results in assessing morphology and function of the kidneys [20] ; however, the risk of gadolinium contrast remains a significant concern in patients with renal insufficiency. Several studies of non–contrast-enhanced MRA have revealed excellent sensitivity in detecting renal artery stenosis. [21] MRA is commonly used in children and pregnant women to avoid the risk of ionizing radiation.
MRA can be complemented with T2 weighting and excretory images after administration of intravenous gadolinium. Multiple acquisitions of static fluid MRIs can ensure adequate visualization of the entire ureter and assess fixed narrowing or obstruction. When contrast is used for MRA, T1-weighted images are used to examine the kidney and vasculature. Intravenous furosemide is used to augment visualization of the excretory system. T1-weighted images are obtained to visualize the bladder for tumors before gadolinium reaches the bladder, as masses can be obscured because of heterogeneous enhancement.
The image quality is less robust with an undistended urinary system. Several interventions such as intravenous fluids, diuretics, compression devices, and gadolinium chelate aid in improving the resolution of MRI. Respiratory and ureteral peristaltic movements may interfere with signal acquisition; however, forced breath-holding may improve the image.
A higher degree of patient cooperation and radiologist supervision is required.
MRI is not very sensitive for detecting calcifications, although renal calculi can be inferred from filling defects or ureteral dilatation.
The sensitivity of MRI in detecting urothelial and kidney malignancies is less well known than with CT imaging.